The medical community continues to strive for advancements in diagnostic technologies, particularly those that can detect pathogens directly from blood samples. A recent session at ASM Microbe 2024 in Atlanta chaired by Linoj Samuel delved into the complexities and challenges that have hindered the integration of these technologies into clinical practice. Direct-from-blood pathogen detection technologies are designed to bypass traditional culture methods, which can be time-consuming and sometimes ineffective in identifying fastidious or non-culturable pathogens. By utilizing such tools, healthcare providers can obtain actionable information swiftly, allowing for the narrowing of therapy and de-escalation of antibiotics. This rapid turnaround is crucial in managing sepsis, where every hour counts in the race against mortality and morbidity.
The session highlighted a blend of technical and non-technical challenges, from the intricacies of sample preparation, pathogen detection to the broader implications for clinical decision-making. Dr. Valeria Fabre’s insightful presentation underscored the potential of these technologies to revolutionize patient care, offering a clinician’s perspective on their impact on treatment strategies.
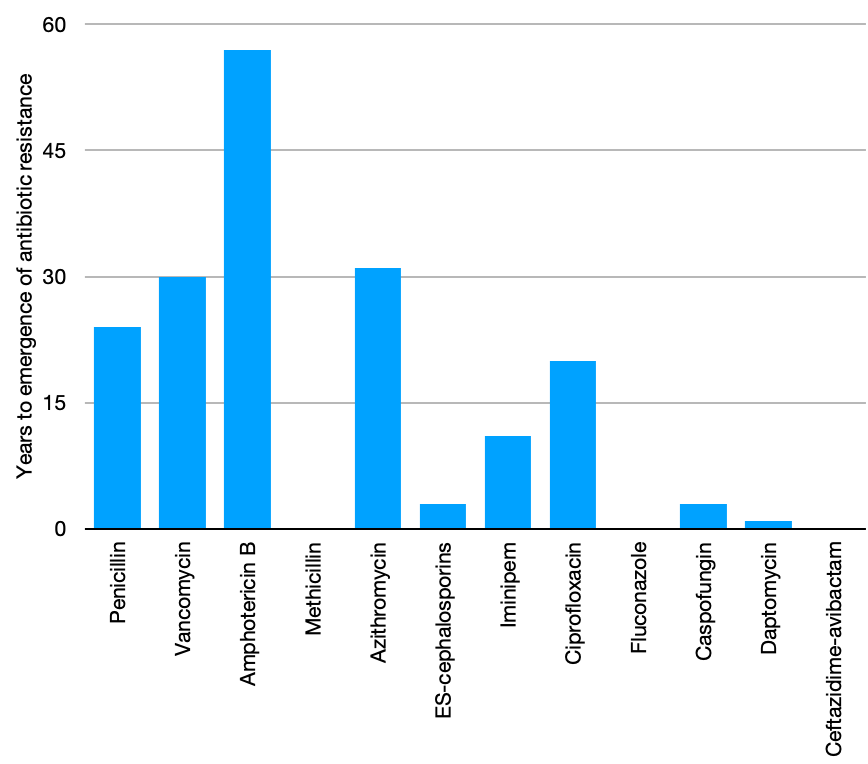
Economically, the implementation of these technologies presents both challenges and opportunities. While initial costs may be higher due to equipment and workforce training, the potential for reducing the length of hospital stays, decreasing the use of broad-spectrum antibiotics, and preventing the spread of resistant pathogens lead to significant savings.
Key takeaways from the discussion emphasized the need for a deeper understanding of the goals behind direct-from-blood pathogen detection. What are the specific outcomes we aim to achieve? How can these technologies influence clinical decisions, patient outcomes, and the economic aspects of healthcare? The current absence of this information hinders assessment of the value such diagnostics bring and thus their adoption. While much of the current efforts are focused on nucleic acid technologies, the development of imaging and spectroscopy-based technologies adds to the diversity of diagnostic approaches, potentially offering complementary benefits to nucleic acid-based methods. These technologies may provide additional layers of information, that may not be available through nucleic acid testing, such as greater confidence in detecting the presence/absence of bacteremia and antimicrobial susceptibility information.
Overall, there is a palpable sense of optimism about the future. The next generation of pathogen detection technologies promises to address current technical limitations more effectively. However, the adoption of these technologies hinges on a much better understanding, and more importantly demonstration, of their value. Failure to take this into account during development and design of validation studies may inhibit their use in clinical settings, which would be a shame.